How to create a gender-responsive pandemic plan
How to create a gender-responsive pandemic plan
Addressing the secondary effects of COVID-19
This tool describes differences in the secondary economic, social, health, and security effects of pandemics across genders. It aims to help decision- makers to address gender disparities in pandemic preparedness, response, and recovery plans.
The tool outlines the process of creating a gender-responsive pandemic plan and priority areas for action; it also provides recommendations on partnership and resources to support stakeholder efforts. This global guidance can be adapted to suit specific contexts and the resources of different actors. The Framework template illustrates how to record related activities and key indicators. By the end of this brief, readers should have a greater understanding of how attention to critical gender-related issues can facilitate development of pandemic plans that are relevant and impactful.
DOWNLOAD A PDF VERSION OF THE TOOL
DOWNLOAD THE BRAZILIAN VERSION OF THE TOOL
DOWNLOAD THE NIGERIAN VERSION OF THE TOOL
DOWNLOAD THE KENYAN VERSION OF THE TOOL
A Gender-Responsive Pandemic Plan takes into consideration the intersectional needs of women, men, and gender minorities, in planning, data collection, response and recovery.
Introduction
Pandemics can have a devastating impact on people, communities, and countries. The experience of those impacts, however, is not uniform. Some groups suffer more acutely than others and struggle more to recover once the virus is contained. To effectively prevent, address and mitigate the differential effects of outbreaks, it is crucial to consider how differences in social characteristics, such as gender, influence not only how pandemics are experienced, but also the efficacy of pandemic control and recovery efforts.
There are gender imbalances in both the primary and secondary effects of pandemics. With respect to primary effects, these include disparities between, and among, women, men, and gender minorities in vulnerability1 2 3 to infection1 4, exposure1 and health outcomes5. In recent disease outbreaks – including Zika in Latin America and the Caribbean, Ebola inWest Africa and the Democratic Republic of Congo, and SARSin Asia – the socioeconomic consequences, or secondary effects, fell disproportionately on more vulnerable members of society, including women and gender minorities6 7. In light of these disparities, failure to take gender into consideration compromises the effectiveness of pandemic responses and puts at risk hard-won gains made towards gender equality.
Developing a gender-responsive pandemic plan must begin with an evaluation of existing gender gaps within a particular context, and assessment of how certain groups may be disproportionately affected. It should encompass pandemic preparedness, response, and recovery. Special attention should be given to gender-based violence; mental health; sexual and reproductive health services; economic and work-related concerns; education and inclusive decision-making. These topics are explored in more depth below.

Examples of gender disparities in secondary effects during the 2020 COVID-19 outbreak
- Work absences in Canada increased more sharply among mothers compared to fathers. From February
to September 2020, the number of mothers who worked less than half their usual hours for reasons likely related to COVID-19 (i.e., caregiving responsibilities, reduced work shifts etc.) increased by 70%, compared to 24% for fathers1. - In the United States, as of July 2020, 79% of heath care personnel infected with COVID-19 were women2.
- Between March and July 2020, calls to the domestic violence helpline in Peru increased by 48%; effect increased over time3.
- Of 1.5 billion students worldwide; UNESCO estimates that more than 11 million girls may not return to school due to the pandemic4.
- Save the Children predicts that 500,000 more girls are at risk of being forced into child marriage in 2020 due to poverty and interruptions in education5.
Data driven response
Data is the basis for developing, implementing, and evaluating an effective gender-responsive pandemic plan. Although gender research and newly emerging findings on COVID-19 effects highlight the differential impacts of pandemics across genders, there remains a global gender data gap that needs to be bridged to mount a stronger, gender-sensitive, COVID-19 response. Ethical and safe collection and analysis of intersectional disaggregated data exposes how pandemics impact groups differently and facilitates realization of appropriate social, economic, and health protections and responses. Available tools and methodologies can guide stakeholders in conducting gender analysis and monitoring gender disparities (see details below under Resources).
Process
A gender-responsive pandemic plan must be multisectoral, multi-step and iterative. Action is needed before, during, and after an outbreak to ensure preparedness, effective response, and optimal recovery. The process of integrating gender considerations into pandemic control is best seen as a continuum rather than three distinct phases. Due to the dynamic nature of pandemics, approaches may change as the disease course evolves; however, the incorporation of gender should remain constant. Throughout this evolving process, it is critical that multilevel, intersectional disaggregated data is collected ethically, and that the data is analyzed, applied, and disseminated to inform evidence-based pandemic planning and implementation.
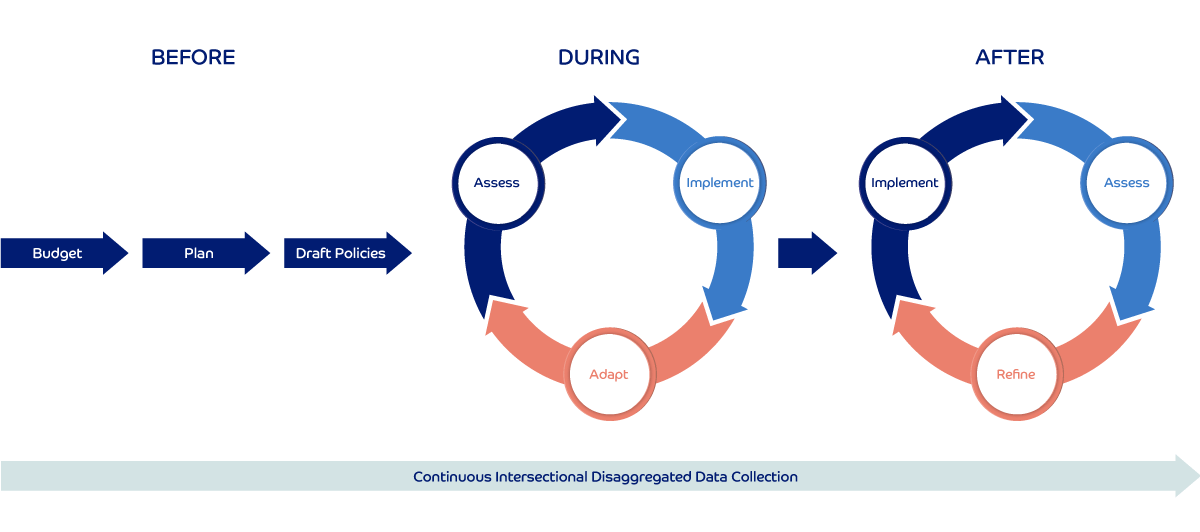
Before: Budget, plan, draft policies
Stakeholders should integrate lessons learned from previous public health emergencies into pandemic preparedness strategies, as well as collect intersectional data, conduct intersectional disaggregated analysis, and monitor indicators of interest to identify priorities and needs. Findings from context-specific gender analyses can then be used to: budget, i.e., determine priorities and decide how to allocate financial and material resources to specific programs and initiatives that target vulnerable groups. Gender budgeting should include established procedures for when and how funding flows will be triggered; stakeholders can then formalize plans for multisectoral program design and activities. This includes agreeing on commitments, outlining specific strategies to integrate gender and reduce inequalities at every stage of pandemic management, and designing a data collection plan to monitor the situation. At this stage leaders should also conduct stakeholder mapping to identify appropriate and representative entities that can implement and oversee response and recovery, and then establish partnerships. Every effort should be made to identify local and grassroots groups that may best represent vulnerable and marginalized populations. Decision-makers may find it prudent to consider the gender impacts of different strategies that may be adopted depending on how the pandemic evolves, and plan accordingly for each possibility. They should also draft policies, i.e., targeted social, economic and health policies should be crafted to protect and support communities in the event of a pandemic. It is important to collaborate meaningfully with gender experts, gender equality advocates and organizations, and representatives of vulnerable groups while developing budgets, plans, and policies.
During: Implement, assess, adapt
This period requires flexibility depending on how far along
one is in establishing a gender-responsive pandemic plan. Those who have taken the preparatory steps outlined in the Before section can respond more quickly and effectively. Less prepared stakeholders should proceed to assess the needs of different groups by undertaking a rapid gender analysis to identify priorities, risks, capacity, and resources to inform strategies for response. More prepared stakeholders can begin by determining which strategies to execute according to the current epidemiological context and conduct a more thorough assessment following implementation of planned activities to monitor both the process and outcomes. As actors implement, they will rollout protective and response interventions in collaboration with multisectoral partners. Clear communication and coordination are critical during this phase, and implementers should institute mechanisms to facilitate these activities. Finally, stakeholders should be prepared to adapt priorities, and planned or initiated activities, based on any new information learned through assessment, as well as inputs from representative partners and groups, to ensure that interventions remain relevant to the current context.

After: Assess, implement, refine
Once disease transmission is under control, stakeholders will need to pivot to recovery and reconstruction as they implement transition planning and maintain support for groups continuing to struggle with the impacts of the pandemic. This stage should also include regular intervals to assess implementation progress and conduct after-action reviews to glean lessons learned from the previous stage. Stakeholders should then refine activities accordingly and record lessons learned for future planning. Decision-makers should also keep in mind that as disease transmission is often nonlinear, they must be prepared to adapt and refine policies and activities as needed once data makes the context clearer, particularly as it applies to vulnerable groups and communities.
Priority areas
Pandemics exert pressure on economic and social systems. In responding to the immediate challenges caused by pandemics, governments have to make difficult decisions about how to best allocate resources. Some of these decisions are necessarily context driven, however, it is also critical to continue to work towards long-term goals and maintain progress that is at great risk of backsliding. The six priority areas summarized below require urgent action to protect against lasting harm to people’s health and wellbeing, and to national economies.
Gender-based violence
Gender-based violence (GBV) can refer to physical, sexual, or psychological coercion and violence. While GBV can be perpetrated against people of all genders, women, and girls (especially adolescents) are more likely to encounter GBV8. According to global estimates, 1 in 3 women (35%) experience some form of physical and/or sexual violence in their lifetime9. GBV experienced by women is often referred to as a ‘hidden’ or ‘shadow’ pandemic, yet even less attention has been paid to another vulnerable group – LGBTQI people experience GBV at rates as high or higher than the general population10 11. The consequences of these experiences are compounded for LGBTQI people who are also often excluded from humanitarian services and resources during disasters12 13.
Data from past emergencies and outbreaks and COVID-19, show increased levels of GBV across contexts compared to before pandemics6 14. Numerous direct and indirect pathways can be linked to this increased violence. Increased economic strain on households, stress, and reduced access to support systems can aggravate GBV. Quarantines and stay-at-home measures can then put vulnerable groups at increased risk of violence15. The risk factors engendered by pandemics are further magnified in fragile settings where power imbalances are more extreme for people dependent on aid for survival who are vulnerable to abuses at the hands of those able to offer assistance. For example, sexual exploitation by community leaders and first responders was reportedly common in Sierra Leone and the Democratic Republic of the Congo during the Ebola crisis15 16.

Mental health
The mental health impacts of pandemics are far-reaching, with many people burdened by fear of infection, social isolation, worry over economic fallout, and grief over personal loss. Studies of past pandemics have outlined the negative psychological impacts of widespread contagion and the resulting socioeconomic fallout and disease prevention measures. Early reports from several countries indicate worse mental health outcomes among the general population since the start of the COVID-19 pandemic. These include increases in drug use, and rates of anxiety and depression17 18 19 20 21 22.
Even before COVID-19, mental health represented a chronically underfunded sector with many countries spending only a fraction of their national health budgets on mental health services. In most countries, mental health services, and community-based services in particular, have been interrupted due to COVID-1923 24. While many countries have implemented telemedicine in response to the disruptions, there is a marked decline in use across high-, middle- and low-income countries. Most high-income countries have reported rolling out these services in contrast to less than half of low-income countries25.
Certain groups are at greater risk of worse mental health outcomes during a public health crisis, including: women overburdened by balancing work, home, and care activities; children, adolescents and older adults struggling with the effects of social isolation; individuals with preexisting mental health conditions; the LGBTQI community; and frontline health workers at increased risk of infection, depression, burnout, and post-traumatic stress26 19 17.
Sexual and reproductive health services
As health systems respond to emergency needs during pandemics, resources are often diverted away from out-patient care, including sexual and reproductive health services for women and girls. Studies and reports from past epidemics in Latin America and the Caribbean, West Africa, and Asia describe how reductions in these essential services during public health crises contributed to increases in unintended pregnancies (including adolescent pregnancy); sexually transmitted infections, including HIV; unsafe abortions; and maternal morbidity and mortality, as well as worse birth outcomes16 6 1. Lack of service delivery due to limited or redirected resources is likely to more severely impact the most vulnerable and marginalized populations who may rely on subsidized care or reside in areas with low human resources for health27.
Women and girls of reproductive age may face many obstacles to accessing sexual and reproductive health services during pandemics, including movement restrictions, lack of affordable childcare, and financial constraints due to unemployment. Supply chain disruptions of essential health commodities (e.g., menstrual health products) and medications, including contraceptives, clearly illustrates the potential ripple effect of conditions produced during pandemics. During the first quarter of 2020, the implementation of public health safety measures in China, a major exporter of pharmaceutical ingredients, delayed production of generic medicines in India. UNFPA estimates that, depending on the level of disruption to the health system during COVID-19, in the event of a 12-month ‘lockdown’ 20-51 million women in 114 low- and middle-income countries will not be able to use modern contraceptives and there will be 6-15 million unintended pregnancies27 28 29.
Although many sexual and reproductive health needs are time sensitive and require intervention from trained providers, women and girls may delay care-seeking during pandemics due to fear of exposure to infection and being misdiagnosed. During the Ebola outbreak in West Africa symptoms of pregnancy complications such as, “unexplained bleeding,” were misclassified as symptoms of Ebola infection and patients were transferred to Ebola treatment centers. Reports from Sierra Leone revealed that women in labor were also reluctant to seek care due to fears that clinicians would not have sufficient personal protective equipment30 29. Facility-based services, including abortion and antenatal, postnatal, and emergency obstetric care need to continue uninterrupted during pandemics, with necessary infection control measures in place31 28 27.
Economic and work-related concerns
Pandemics place millions of jobs at risk; however, certain groups are more vulnerable to the economic and work-related concerns that stem from market contractions and resulting losses in income. Groups disproportionately disadvantaged during pandemics include workers without social protection in the event of unemployment (e.g., self-employed, part-time, informal workers etc.); migrant workers who may also lack legal immigration status; and women, many of which are racial and ethnic minorities, who are overrepresented in the more adversely affected sectors32. Women are also on the front lines of the current COVID-19 pandemic – in the health and social workforce where they represent 70% of paid employees, and at home, where they carry out more of the unpaid care work33. Their risk of infection during pandemics can be further compounded by context specific power dynamics. During the 2014 Ebola crisis in West Africa there were reports that in clinical settings men, who comprised the majority of higher-ranking staff (i.e., doctors), received more personal protective equipment than women in lower ranking positions (i.e., nurses, traditional birth attendants, community health workers etc.)16.
Livelihoods
Vulnerable groups tend to be overrepresented in certain types of work. In many countries, specific sectors (i.e., tourism, travel, retail, services etc.), in which women generally constitute the majority, tend to be more vulnerable to pandemic control measures32 34 16. According to the US Labor Department, women accounted for approximately 60% of the 700,000 jobs lost in the first COVID-19 wave – a trend observed in multiple other countries since the start of the pandemic35 36. The global garment industry which is 75% women, has also been devastated by the COVID-19 pandemic, with laborers losing income as factories suspend or lay off employees. These workers are more likely to be subject to acute economic loss from the immediate disruption of their work. Those who continue to work generally lack social protections (e.g., paid sick leave) and may be at increased risk of infection due to close working quarters or the nature of their work37 16. Adverse economic outcomes run the risk of pushing people and households into multidimensional poverty. UN Women estimates that by 2021, 96 million more people will be forced into extreme poverty, and the gender poverty gap will expand34. Globally, women are also more likely to live in poor households with underage dependents. Women and girls in lower-income settings may be disproportionately impacted by some of the consequences of compromised livelihoods, such as early marriage and food insecurity16.

Informal work sector
The 2-billion-person global informal workforce is another sector differentially affected by disease outbreaks. It was one of the hardest hit during the COVID-19 pandemic. During the first month of the pandemic, estimates suggest that globally informal workers, many of which are from minority populations, lost an average of 60% of their income34. Although it varies, in most countries, women are employed in the majority of informal work positions such as domestic work; 72% of domestic workers worldwide, 80% of whom were women, lost jobs due to the COVID-19 pandemic34. In addition to the loss of income, often informal workers are not covered by unemployment or health plans putting them in the unenviable position of choosing between returning to work early despite the risks to their health and being unable to meet their basic needs for survival38.
Unpaid care work
Care work is historically undervalued, uncompensated, and frequently excluded from formal social protection16. According to the UN, even before COVID-19, on an average day women did three times as much unpaid care and domestic work as men. During pandemics, domestic work generally increases for women, including those who already have full-time jobs28. Often, confinement and infection control measures (e.g., school closures) further compound the burden of unpaid care work that tends to fall to women and girls28 39 37 1 40. This can have many consequences, including limiting their ability to continue their studies, carry out paid work, and even in some cases return to the labor market after an outbreak1 41.
Representation and valuing diverse voices
In 2019, the World Health Organization declared that global health is delivered by women and led by men33. Women account for 70% of the global social and health workforce and yet they hold a mere 25% of senior roles33. Gender parity could help to expand global heath priorities and to make them more inclusive. Given their marked majority in the workforce, and disproportionate risk to certain impacts of pandemics, women constitute an undeniably important group of stakeholders. Decision-makers should demonstrate a greater commitment to representation and valuing diverse voices, including underrepresented minorities, in local, national, and global leadership positions. While important, increased representation is not enough to advance gender equality in global health governance. Commitment to changing informal practices that may hinder certain groups’ participation (e.g., inflexible work hours disadvantage mothers)42 and exploit existing gender norms (e.g., men’s lack of involvement in unpaid care work) is also key43 44.
Exclusion and lack of meaningful participation also threatens the success of public health interventions. For example, due to their embeddedness in local communities, networks of women and young people are often ideally positioned to receive and communicate important information on detection, prevention, treatment, and social support45 43. It is also important to consider how certain policy landscapes can enable better pandemic preparedness and response. There has been much public discourse, and some limited evidence, suggesting that women in leadership positions have more successfully managed public health crises. Lower rates of infection and death in some woman-led states during the first quarter of the COVID-19 pandemic gave rise to speculation that gender differences in leadership and risk management styles might explain women’s relative success in this context (i.e. several women leaders adopted ‘lockdown’ policies early in the pandemic)46. However, more nuanced scholarship that considers leadership in the context of national systems of governance and cultural values suggests that successful pandemic management was less the result of leaders’ gender than the fact that some woman-led states already had protocols in place that allowed their leaders to respond more quickly and effectively to COVID-19. In these cases, the same political and social values that motivated countries to prioritize strong disaster management systems contributed to their selection of women for positions of national leadership47

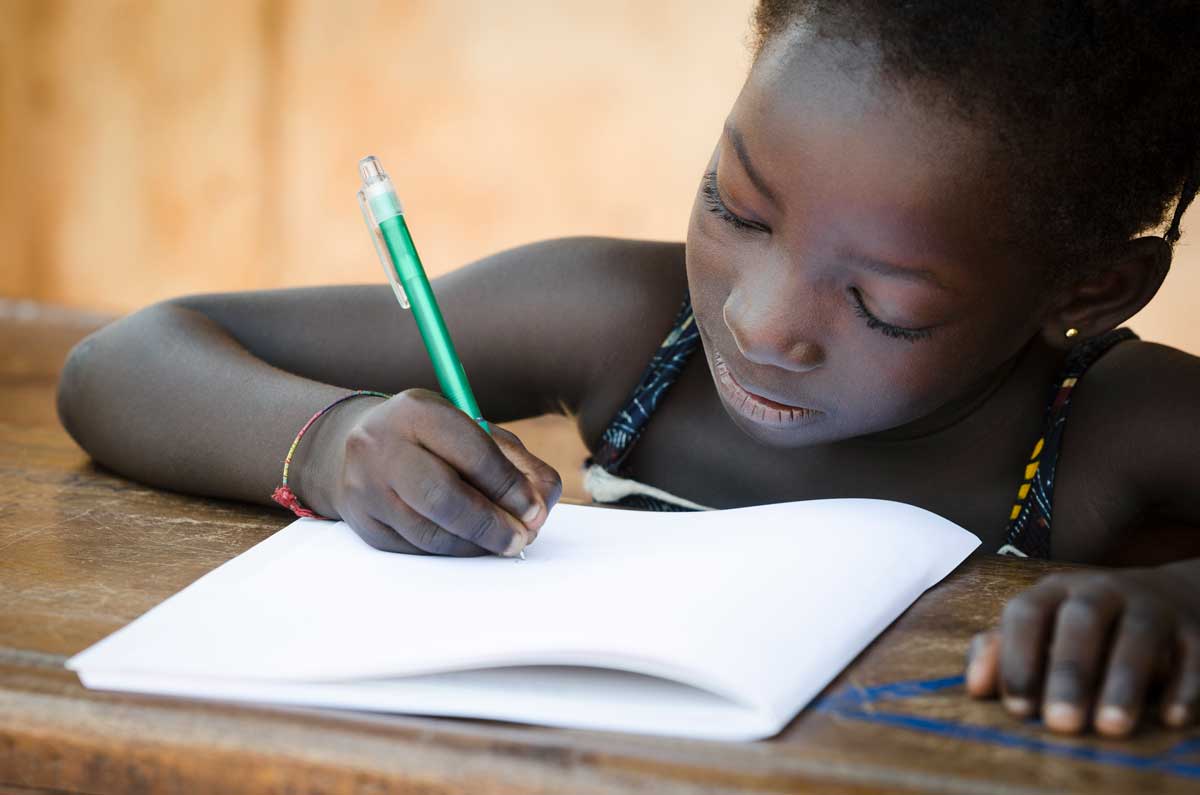
Education
During pandemics, education for adolescents and children requires special protection. In addition to delivering learning opportunities, schools also perform many other important social services, including functioning as safe places for reporting abuse, dispensing free or low-cost reproductive health supplies (i.e., condoms, sanitary napkins), providing social structures critical to healthy development, and supplying free or subsidized meals for underprivileged students48. Policy responses to the COVID-19 pandemic have disrupted education for hundreds of millions of students from every continent around the world. A rapid assessment of education needs in 98 countries found that without intervention, the lost opportunities to learn, and disparities in the ability of households and schools to support remote learning during the COVID-19 pandemic, would likely lead to “the greatest disruption in educational opportunity worldwide in a generation”49 50. These disruptions come at a high cost in the short-term, and the ripple effects may negatively impact individual livelihoods within communities for years to come.
Pandemics expose inequities across the education sector and they also have the potential to widen existing disparities in educational achievement51 52. During the 2014-16 Ebola outbreak in West Africa, some struggling households turned to children to contribute to the family income rather than focusing on school. Girls were also often expected to take on additional caregiving tasks within the home, limiting learning opportunities for them during the pandemic, and increasing rates of attrition after the crisis39 16 53 54. School attrition has serious downstream social consequences, including less economic earning power over a lifetime; girls who do not complete school are also more vulnerable to decreased agency at the household and societal level throughout their lifespan. Ample evidence shows that economic insecurity puts adolescent girls at increased risk of abuse and sexual exploitation, including early and forced marriage and early pregnancy, further reducing the likelihood that they will return to school16 39 51 55 54.
In addition to girls, refugees, and learners with disabilities, students living in resource-poor or rural areas are at a particular disadvantage as school closures reduce learning opportunities. Parents who have limited education, or need to work, may not be able to effectively facilitate remote learning for their children. Low- and middle-income countries and communities with limited internet connectivity may be ill-equipped to support distance learning, and gender gaps in access to digital devices and the information communication technology skills necessary for online education can lead to learning disparities between boys and girls53 39 51.
Partnerships
Partnerships and collaboration are essential to a successful gender-responsive pandemic plan. Governments, non-governmental organizations, international organizations, the private sector, and civil society all have important roles to play before, during, and after pandemics, and a shared responsibility to find and execute effective solutions. Pandemic impacts are not limited to the health sector, they require multisectoral action. Failure to collaborate across sectors can lead to service gaps or overlapping activities.
Benefits of partnership
- Share responsibility
- Avoid duplication
- Increase awareness
- Expand reach
- Pool resources
- Enhance community buy-in
- Leverage cross-sectoral expertise and combine strengths
Gender refers to the socially constructed roles, norms, and behaviors we associate with men, women, and gender minorities. Expectations and implications of gender are shaped by historical and cultural context and intersect with other facets of identity (e.g., ethnicity or sexual orientation) to influence how people experience life.
Intersectionality is a theoretical framework that examines how people’s experiences of discrimination and privilege are influenced by the combined aspects of their social identity. An example of intersectional disaggregated data would therefore be data broken down by age, sex, gender, race, class, disability, sexual orientation, and related combinations.
Shared responsibility also has the benefit of mitigating the risk of overwhelming any one sector. Furthermore, plans to prevent and address the effects of an outbreak may be so interrelated that even by simply engaging in independent action, one sector (e.g., health, education, economy) may contribute to the objectives of another. For example, provision of sexual and reproductive health services during a pandemic can help to prevent unplanned teenage pregnancies that may make it more difficult for adolescent girls to return to school, leaving them more vulnerable to poverty throughout their lifetime56. Given the complexity of intersectoral collaboration, appointing a dedicated unit to manage strategic coordination and communication is advisable. Appointed bodies can also ensure general oversight and participatory and transparent processes.
Partnerships can be forged at different levels from the local to the national and the international level. To identify which level to target, the jurisdiction under which a given policy or program of interest falls should be considered. Depending on the context, federal-level partnerships may have a wider influence and impact, while local-level partnerships may be more accessible to civil society and public services (e.g., first responders). Civil society partners frequently have more insight into the cultural and socioeconomic realities on the ground and are often already involved in providing critical social services. They can also play an important role in enhancing community support, which is essential to successful adoption of social and health prevention, protection, and promotion efforts. Such partners include community-based organizations (e.g., women’s groups), humanitarian organizations, and community leaders (e.g., religious institutions, employers, local government, traditional leaders etc.). Community-based members of the public sector, like community health workers, should also be an integral part of any gender-responsive pandemic plan.
A number of activities are prerequisite to partnership development, including mapping key stakeholders; identifying champions; and assessing each stakeholder’s interests, constraints, and scope of authority. Understanding how different parties are positioned helps to enable identification of common ground. Both formalized groups and informal channels on digital messaging platforms etc. can facilitate communication among various actors. Information and data sharing among partners are also essential to breaking down silos and ensuring a coordinated and data-driven response to pandemics. Stakeholders should be mindful that the composition of partnerships and the level of engagement of partners may change over the course of a pandemic, as a result it is important to communicate roles, responsibilities, and time frames clearly.
Resources
This curated selection of resources provides detailed guidance and materials to support stakeholders in incorporating gender into the various stages of pandemic plans.
- The Jhpiego Gender Analysis Toolkit provides research questions for project-level data collection and gender analysis related to five domains: 1) Laws, regulations, and institutional practices; 2) Cultural norms and beliefs; 3) Gender roles, responsibilities, and time used; 4) Access to and control over assets and resources; and 5) Patterns of power and decision-making.
- The Gender Analysis and COVID-19 Matrix provides a template and examples to guide development of a framework that factors multidimensional gender-related considerations into the design of research and/or interventions.
- A WHO Toolkit provides guidance for infectious disease researchers on how to incorporate an intersectional gender approach into their work.
- The One Health Gender Integration Toolkit contains guidance on how to identify and manage gender considerations related to preparedness and response to public health threats. The Toolkit includes supporting tools for gender-related disease prevention, detection, and response as well as analysis.
- A WHO critical review of 17 tools widely used for Gender Analysis in Health describes the purpose, content, and limitations of each tool. It also includes full references for each of the tools reviewed.
Framework
The Gender-Responsive Pandemic Plan Framework outlines illustrative activities that can be implemented to achieve desired outcomes for each of the Priority Areas described in the brief. Examples are illustrative only. Actual activities and indicators will need to be adapted according to the context of a given pandemic and the resources available to actors. Key activities that can be taken before, during, and after an outbreak are listed; the Framework also indicates that ethical intersectional disaggregated data collection is an ongoing activity that should be conducted across all three stages. Examples of key indicators, some of which are adapted from the UN Sustainable Development Goals global indicator framework, for each outcome are also included.
| Outcomes | Key Activities | Indicators | ||
|---|---|---|---|---|
| Before | During | After | ||
| Address gender-based violence |
|
|
|
|
|
||||
| Provide mental health support |
|
|
|
|
|
||||
| Ensure access to sexual and reproductive health services |
|
|
|
|
|
||||
| Address economic and work-related concerns |
|
|
|
|
|
||||
| Ensure equitable and meaningful representation in decision makin |
|
|
|
|
|
||||
| Ensure equitable access to education |
|
|
|
|
|
||||
1This indicator is especially hard to track during a pandemic, as it may be unsafe to survey people during confined to their homes. Also, the turnaround time for such surveys is long. During the COVID-19 pandemic GBV has been measured using proxy indicators such as the number of hotline calls and police reports, etc. Additional sources of information include reports from civil society organizations, shelters, community health workers, child services providers, and other groups that have historically not been consulted in data collection.
Acknowledgements
This brief was developed by representatives from the Gender and COVID-19 Project. The authors would like to express their sincere thanks to the following reviewers (listed alphabetically by last name) for their feedback and contributions to this brief: Jashodhara Dasgupta, SAHAYOG, India; Sandra MacDonald, University of Northampton, UK; Megan O’Donnell, Center for Global Development, USA; Ateeb Ahmad Parray, BRAC James P Grant School of Public Health, BRAC University, Bangladesh; Amber Peterman, University of North Carolina at Chapel Hill, USA; Niyati Shah, World Bank, USA; Gilla Shapiro, Princess Margaret Cancer Centre at the University of Toronto Health Network, Canada; Alexandra Solomon, Independent Researcher, USA; Sylvie Grace Taylor Armstrong, European University Institute, Italy.
Authors
Erica N. Rosser, Rosemary Morgan, Heang-Lee Tan, Kate Hawkins, Anne Ngunjiri, Amy Oyekunle, Brunah Schall, Denise Nacif Pimenta, Eduardo Tamaki, Mariela Rocha, Clare Wenham
Contact
For additional information, please contact the Gender and COVID-19 Project: genderandcovid-19.org/contact
Suggested citation
Rosser EN, Morgan R, Tan H, Hawkins K, Ngunjiri A, Oyekunle A, Schall B, Nacif Pimenta D, Tamaki E, Rocha M and Wenham C. (2021) “How to Create a Gender-Responsive Pandemic Plan: Addressing the Secondary Effects of COVID-19.” Gender and COVID-19 Project. genderandcovid-19.org
References
- World Health Organization. (2020). Gender and COVID-19: advocacy brief, 14 May 2020. World Health Organization. https://apps.who.int/iris/handle/10665/332080
- Gabriel, G., & Arck, P. C. (2014). Sex, Immunity and Influenza. Journal of Infectious Diseases, 209(suppl 3), S93–S99. https://doi.org/10.1093/infdis/jiu020
- World Health Organization Regional Office for the Western Pacific. (2011). Taking sex and gender into account in emerging infectious disease programme : An analytical framework. https://www.who.int/publications/i/item/9789290615323
- Wingfield, T., Cuevas, L. E., MacPherson, P., Millington, K. A., & Bertel Squire, S. (2020). Tackling two pandemics: a plea on World Tuberculosis Day. The Lancet, 8(June), 536–538. https://doi.org/10.1016/S2213-2600(20)30232-0
- Harvard GenderSci Lab. (2020). US Gender/ Sex COVID-19 Data Tracker — GenderSci Lab.
https://www.genderscilab.org/gender-and-sex-in-covid19 - Wenham, C., Smith, J., Davies, S. E., Feng, H., Grépin, K. A., Harman, S.,Herten-Crabb, A., & Morgan, R. (2020). Women are most affected by pandemics – lessons from past outbreaks. Nature, 583(7815), 194–198.
https://doi.org/10.1038/d41586-020-02006-z - UN Women. (2020). Gender-Responsive Prevention and Management of the COVID-19 Pandemic: From Emergency Response to Recovery & Resilience.
https://www.unwomen.org/ - UNICEF. (2020). Gender-Based Violence in Emergencies. https://www.unicef.org/protection/gender-based-violence-in-emergencies
- World Health Organization. (2017). Violence against Women. World Health Organization. http://www.who.int/news-room/fact-sheets/detail/violence-against-women
- Rollè, L., Giardina, G., Caldarera, A. M., Gerino, E., & Brustia, P. (2018). When Intimate Partner Violence Meets Same Sex Couples: A Review of Same Sex Intimate Partner Violence. Frontiers in Psychology, 9(1506).
https://doi.org/10.3389/fpsyg.2018.01506 - Human Rights Campaign. (2015). Sexual Assault and the LGBTQ Community. HRC. http://www.hrc.org/resources/sexual-assault-and-the-lgbt-community
- Gaillard, J. C., Gorman-Murray, A., & Fordham, M. (2017). Sexual and gender minorities in disaster. Gender, Place & Culture, 24(1), 18–26.
https://doi.org/10.1080/0966369x.2016.1263438 - Dominey-Howes, D., Gorman-Murray, A., & McKinnon, S. (2016). Emergency management response and recovery plans in relation to sexual and gender minorities in New South Wales, Australia. International Journal of Disaster Risk Reduction, 16, 1–11.
https://doi.org/https://doi.org/10.1016/j.ijdrr.2016.02.004 - Peterman, A., & O’Donnell, M. (2020). COVID-19 and Violence against Women and Children: A Second Research Round Up. Center For Global Development.
https://www.cgdev.org/publication/covid-19-and-violence-against-women-and-children-second-research-round - Peterman, A., Potts, A., O’Donnell, M., Thompson, K., Shah, N., Oertelt-Prigione, S., & van Gelder, N. (2020). Pandemics and Violence Against Women and Children (No. 528). https://www.cgdev.org/publication/pandemics-and-violence-against-women-and-children
- The World Bank. (2020). Gender Dimensions of the COVID-19 Pandemic (English). World Bank Group. https://documents.worldbank.org/en/publication/documents-reports/documentdetail/618731587147227244/gender-dimensions-of-the-covid-19-pandemic
- Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., Barger, L. K., Czeisler, C. A., Howard, M. E., & Rajaratnam, S. M. W. (2020). Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. In MMWR. Morbidity and Mortality Weekly Report (Vol. 69, Issue 32). Centers for Disease Control MMWR Office.
https://doi.org/10.15585/mmwr.mm6932a1 - McGinty, E. E., Presskreischer, R., Han, H., & Barry, C. L. (2020). Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA, 324(1), 93–94. https://doi.org/10.1001/jama.2020.9740
- Talevi, D., Socci, V., Carai, M., Carnaghi, G., Faleri, S., Trebbi, E., Di Bernardo, A., Capelli, F., & Pacitti, F. (2020). Mental Health Outcomes of the CoViD-19 Pandemic. Rivista Di Psichiatria, 55(3), 137–144. https://pubmed.ncbi.nlm.nih.gov/32489190/
- Dong, L., & Bouey, J. (2020). Public Mental Health Crisis during COVID-19 Pandemic, China. Emerging Infectious Diseases, 26(7), 1616–1618. https://doi.org/10.3201/eid2607.200407
- Vindegaard, N., & Benros, M. E. (2020). COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity, 89, 531–542. https://doi.org/https://doi.org/10.1016/j.bbi.2020.05.048
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet, 395(10227).
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30460-8/fulltext - World Health Organization. (2020, October 5). COVID-19 disrupting mental health services in most countries, WHO survey. WHO News Release. https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey
- World Health Organization. (2020, May 14). Substantial investment needed to avert mental health crisis. WHO News Release. https://www.who.int/news/item/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis
- World Health Organization. (2020). The impact of COVID-19 on mental, neurological and substance use services : results of a rapid assessment. (p. 36). World Health Organization. https://www.who.int/publications/i/item/978924012455
- Dean, L., Cooper, J., Wurie, H., Kollie, K., Raven, J., Tolhurst, R., MacGregor, H., Hawkins, K., Theobald, S., & Mansaray, B. (2020). Psychological resilience, fragility and the health workforce: lessons on pandemic preparedness from Liberia and Sierra Leone. BMJ Global Health, 5(9), e002873. https://doi.org/10.1136/bmjgh-2020-002873
- Ahmed, Z., & Sonfield, A. (2020). The COVID-19 Outbreak: Potential Fallout for Sexual and Reproductive Health and Rights. Guttmacher Institute. https://www.guttmacher.org/article/2020/03/covid-19-outbreak-potential-fallout-sexual-and-reproductive-health-and-rights
- UNFPA. (2020). COVID-19: A Gender Lens, Protecting Sexual and Reproductive Health and Rights, and Promoting Gender Equality. https://www.unfpa.org/resources/covid-19-gender-lens
- UNFPA. (2020). Impact of the COVID-19 Pandemic on Family Planning and Ending Gender-based Violence, Female Genital Mutilation and Child Marriage | UNFPA – United Nations Population Fund. UNFPA. https://www.unfpa.org/resources/impact-covid-19-pandemic-family-planning-and-ending-gender-based-violence-female-genital
- Chattu, V. K., & Yaya, S. (2020). Emerging infectious diseases and outbreaks: implications for women’s reproductive health and rights in resource-poor settings. Reproductive Health, 17(1), 43. https://doi.org/10.1186/s12978-020-0899-y
- UN Women. (2020). The Impact of COVID-19 on Women. UN Women. https://www.unwomen.org/-/media/headquarters/attachments/sections/library/publications/2020/policy-brief-the-impact-of-covid-19-on-women-en.pdf?la=en&vs=1406
- International Labor Organization. (2020). COVID-19 and World of Work: Impact and policy responses. In ILO Monitor (1st ed.). International Labour Organisation. www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/documents/briefingnote/wcms_738753.pdf
- World Health Organization. (2019). Delivered by women, led by men: A gender and equity analysis of the global health and social workforce. In Human Resources for Health Observer Series;24. World Health Organization. https://apps.who.int/iris/handle/10665/311322
- Azcona, G., Bhatt, A., Encarnacion, J., Plazaola-Castaño, J., Seck, P., Staab, S., & Turquet, L. (2020). From Insights to Action: Gender Equality in the Wake of COVID-19. UN Women. http://www.unwomen.org/en/digital-library/publications/2020/09/gender-equality-in-the-wake-of-covid-19
- Madgavkar, A., White, O., Mahajan, D., Azcue, X., & Krishnan, M. (2020, July 15). COVID-19 and Gender Equality: Countering the Regressive Effects. McKinsey Featured Insight. http://www.mckinsey.com/featured-insights/future-of-work/covid-19-and-gender-equality-countering-the-regressive-effects#
- Horsley, S. (2020, April 8). Women Are Losing More Jobs In Coronavirus Shutdowns. NPR. https://www.npr.org/2020/04/08/829141182/women-are-losing-more-jobs-in-coronavirus-shutdowns?t=1608652026655
- CARE. (2020). What Is the Impact of COVID-19 on the Global Garment Industry? https://www.careinternational.org.uk/what-impact-covid-19-global-garment-industry
- ACAPS. (2020). Global Gender Analysis, COVID-19: Impact on gender dynamics in the livelihoods sector within crisis-affected countries. ACAPS. https://www.acaps.org/special-report/global-gender-analysis-covid-19-and-livelihood
- Briggs, H., Haberland, N., De Hoop, T., Ngo, T. D., & Desai, S. (2020). The Impact of COVID-19 on Opportunities for Adolescent Girls and the Role of Girls’ Groups. Evidence Consortium on Women’s Groups. https://www.air.org/sites/default/files/Adolescent-Girls-COVID-Brief-Sept-2020.pdf
- UN Women. (2020). COVID-19: Emerging Gender Data and Why It Matters. UN Women Data Hub; UN Women. https://data.unwomen.org/resources/covid-19-emerging-gender-data-and-why-it-matters
- UN Women. (2020). Whose Time to Care? Unpaid Care and Domestic Work During Covid-19. UN Women. https://data.unwomen.org/sites/default/files/inline-files/Whose-time-to-care-brief_0.pdf
- 42. Davies, S. E., Harman, S., Manjoo, R., Tanyag, M., & Wenham, C. (2019). Why it must be a feminist global health agenda. The Lancet, 393(10171), 601–603.
https://doi.org/10.1016/s0140-6736(18)32472-3 - UNICEF. (2020). Five Actions for Gender Equality in the COVID-19 Response. UNICEF. https://www.unicef.org/documents/five-actions-gender-equality-coronavirus-disease-covid-19-response-technical-note
- Harman, S. (2016). Ebola, gender and conspicuously invisible women in global health governance. Third World Quarterly, 37(3), 524–541. https://doi.org/10.1080/01436597.2015.1108827
- Meagher, K., Singh, N. S., & Patel, P. (2020). The role of gender inclusive leadership during the COVID-19 pandemic to support vulnerable populations in conflict settings. BMJ Global Health, 5, 3760. https://doi.org/10.1136/bmjgh-2020-003760
- Garikipati, S., & Kambhampati, U. (2020). Leading the Fight Against the Pandemic: Does Gender “Really” Matter? SSRN. https://dx.doi.org/10.2139/ssrn.3617953
- Windsor, L. C., Yannitell Reinhardt, G., Windsor, A. J., Ostergard, R., Allen, S., Burns, C., Giger, J., & Wood, R. (2020). Gender in the time of COVID-19: Evaluating national leadership and COVID-19 fatalities. PLOS ONE, 15(12), e0244531. https://doi.org/10.1371/journal.pone.0244531
- UNESCO. (2020). Adverse Consequences of School Closures. UNESCO. http://en.unesco.org/covid19/educationresponse/consequences
- Reimers, F. M., & Schleicher, A. (2020). A framework to guide an education response to the COVID-19 Pandemic of 2020. OECD. https://globaled.gse.harvard.edu/files/geii/files/framework_guide_v2.pdf
- UNESCO. (2020, August 28). COVID-19: UNESCO and Partners in Education Launch Global Campaign to Keep Girls in the Picture. UNESCO. http://en.unesco.org/news/covid-19-unesco-and-partners-education-launch-global-campaign-keep-girls-picture
- UN. (2020). Education during COVID-19 and beyond. UN. https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf
- Schleicher, A. (2020). The impact of covid-19 on education: Insights from education at a glance 2020. Organisation for Economic Co-operation and Development. https://www.oecd.org/education/the-impact-of-covid-19-on-education-insights-education-at-a-glance-2020.pdf
- UNESCO. (2020). Addressing the Gender Dimensions of COVID-Related School Closures: Vol. 3.1. UNESCO. http://unesdoc.unesco.org/ark:/48223/pf0000373379
- UNICEF, & International Rescue Committee. (2020). COVID-19: GBV Risks to Adolescent Girls and Interventions to Protect and Empower them. In www.unicef.org. UNICEF. https://www.unicef.org/media/68706/file/COVID-19-GBV-risks-to-adolescent-girls-and-interventions-to-protect-them-2020.pdf
- UNESCO. (2020). Keeping Girls in the Picture. UNESCO. en.unesco.org/covid19/educationresponse/girlseducation
- Kuruvilla, S., Hinton, R., Boerma, T., Bunney, R., Casamitjana, N., Cortez, R., Fracassi, P., Franz-Vasdeki, J., Helldén, D., McManus, J., Papp, S., Rasanathan, K., Requejo, J., Silver, K. L., Tenhoope-Bender, P., Velleman, Y., Wegner, M. N., Armstrong, C. E., Barnett, S., … Graham, W. (2018). Business not as usual: how multisectoral collaboration can promote transformative change for health and sustainable development. BMJ, 363(k4771), 1–10. https://doi.org/10.1136/bmj.k4771
Text box citations
- Canada Statistics. (n.d.). Labour Force Survey, September 2020. In The Daily. https://www.statcan.gc.ca/eng/start
- Hughes, M. M., Groenewold, M. R., Lessem, S. E., Xu, K., Ussery, E. N., Wiegand, R. E., Qin, X., Do, T., Thomas, D., Tsai, S., Davidson, A., Latash, J., Eckel, S., Collins, J., Ojo, M., McHugh, L., Li, W., Chen, J., Chan, J., … Stuckey, M. J. (2020). Update: Characteristics of Health Care Personnel with COVID-19 — United States, February 12–July 16, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(38), 1364–1368. https://doi.org/10.15585/mmwr.mm6938a3
- Agüero, J. M. (2020). COVID-19 and The Rise of Intimate Partner Violence. World Development, 137(105217). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7522673/
- UNESCO. (2020, August 28). COVID-19: UNESCO and Partners in Education Launch Global Campaign to Keep Girls in the Picture. UNESCO. https://en.unesco.org/news/covid-19-unesco-and-partners-education-launch-global-campaign-keep-girls-picture
- Cousins, S. (2020). 2·5 million more child marriages due to COVID-19 pandemic. The Lancet, 396(10257). https://doi.org/10.1016/s0140-6736(20)32112-7